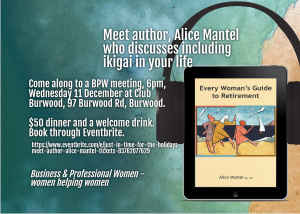
Introducing Every Woman’s Guide to Retirement
Author: Alice Mantel
Virus closes arts events
Following government announcements, many major arts events are now cancelled due to fears of the Covid-19 virus spreading through large public gatherings.
Amongst the cancelled performances are the Sydney Writers’ Festival, the Royal Easter Show, the Byron Bluesfest and the Festival of Dangerous Ideas. Other large events that have been cancelled include the Parramatta multicultural festival and the Blue Mountains Music Festival.
While these steps are acknowledged to be quite extreme, organisations have followed government directives to restrict non-essential gatherings to less than 500 people to reduce any possible transmission from close contacts. Football and cricket games have also been impacted and will be played inside a “silent” stadium.
NSW hospital are implementing contingency plans to deal with the expected influx of cases after 14 new coronavirus cases were confirmed in NSW over the last weekend. Most of these cases were associated with travellers returning to Australia. Aged care facilities have been given specific guidelines asking family and friends to limit their visits to relatives to reduce the likelihood of infection.
To date, five deaths and 368 confirmed cases due to the coronavirus have been recorded in Australia. It is not known how long these new restrictions will apply.
Relax while you plan your retirement
Branch out and join the retirement conversation
Skills-based volunteering can boost your career prospects
Although this article is written from the perspective of a new graduate, its advice is equally applicable to older people looking for work in this tough employment market.
From giving back to the community to learning new professional skills, GradConnection shares the reasons why you should volunteer – and why a good volunteer role is far more important than just a line on your resume.
As any recent graduate or anyone approaching the end of their university studies knows, the market for graduate jobs is increasingly competitive. In 2019, the ABC reported that the year prior, only 73 per cent of Australian graduates found full-time employment in their field within four months of graduation. Citing research from Universities Australia, the ABC also reported that since the 2008 global financial crisis, the period between graduation and securing long-term employment has lengthened.
Against this backdrop, many graduates are exploring the advantages of volunteering in terms of not only personal development, but helping their resumes and applications stand out. Whether you’re considering working with a small community group or larger not-for-profit organisation, studies have shown that the benefits of volunteering include an increased perception of employability among potential employers.
Here are some of the professional and personal benefits of volunteering:
- You’ll develop greater interpersonal skills
Whether you’re joining a small grassroots organisation or an established charity, participating in volunteer work is a great way to sharpen your people skills. Learn how to communicate effectively with people from all walks of life, and develop greater empathy and teamwork skills that will serve you in the early years of your career and beyond.
Beyond teaching you how to empathise with people from different backgrounds, there’s also considerable evidence to suggest that volunteering is good for your health. Volunteer work can make you feel like part of a community and give you a sense of purpose and achievement, all of which can contribute to improved overall mental health. What’s more, all the communication skills you learn in a volunteer job can later be applied in full time employment.
- You’ll learn how to be flexible
Other key advantages of volunteer work are the flexibility and resilience it will encourage you to develop. As many charitable and community organisations have a lean staff, they often rely heavily on volunteer contributions to keep things running. In many cases, this will require you to be flexible and quickly adapt to changing deadlines and priorities.
Rather than seeing this as a challenge, think of it as valuable work experience: Even in full-time work, things don’t always go as planned, and the ability to keep a cool head and think on your feet is highly valuable.
- You’ll gain experience in a range of roles
In addition to flexibility, the benefits of volunteering extend to exposure to a range of roles. Similar to internships or clerkships that operate on a rotation basis, volunteer work can give you valuable, practical experience in a range of different positions.
For example, you might assist with marketing one day and help plan a fundraising event the next. The close, tight-knit environment of many organisations that benefit from volunteering makes them the perfect environment in which to develop new skill sets. Having a diverse range of skills can ultimately help you find a graduate job in your dream industry, and make you a valuable all-rounder addition to any team.
- You’ll make a habit of giving back
Arguably one of the biggest perks of volunteering is the knowledge that you’re giving back and contributing in a meaningful way to the wider community. The benefits of volunteering for the community are clear, wherever you choose to donate your time. Whether you’re working at a community legal centre, soup kitchen, or environmental organisation, volunteer work is a fantastic way to support the less fortunate and those in a difficult stage of their life.
Employers are also keenly aware of the personal benefits of volunteering for the community, and see many of the resulting traits as highly desirable. Research by SEEK Volunteer found that for many prospective employers, applicants with volunteering experience were perceived as motivated, proactive, and socially responsible – and therefore eminently more valuable.
Pro Tip: Don’t overlook the importance of volunteering
For 92 per cent of Australian employers, relevant volunteer experience gives candidates a significant competitive advantage. So what are you waiting for? Now that you know the professional and personal benefits of volunteering, it’s time to get out there and start helping your community.
How to be happier, even when you’re not
Christmas can be a stressful time of year. You will blow your budget, your relatives will annoy you, and you’ll receive gifts that go straight to Vinnies, all in 40℃ heat.
Meanwhile, your friends post pictures on social media of their idyllic vacations, yearly accomplishments, and super happy toddlers and cats. You may feel extra stress from not accomplishing all the goals you set at the start of the year. You feel this stress in the face of other people’s overt jolliness.
So how can the science of gratitude help you not only cope with, but enjoy, the ups and downs of the festive season?
Remind me again, what is gratitude?
Gratitude, in short, is a strong feeling of appreciation towards someone who’s helped you. You can also feel gratitude when you make a habit of noticing and appreciating the positives in life. This might be feeling grateful for a cooling breeze on a hot day, appreciating your abilities in the kitchen or as a good friend.
Over the past 20 years or so, there has been quite a bit of research on gratitude.
Some of our own research shows older people are more grateful than younger people; suggests gratitude serves an evolutionary purpose by helping humans bond; and shows it’s possible to become more grateful with practice.
How can gratitude help me?
Practising gratitude often can have many positive impacts, including: an increased sense of well-being and life satisfaction; positive emotional functioning such as more pleasurable emotions and thoughts that life is going well; increased optimism; a sense of connectedness; improved relationships; and more and better quality sleep.
So all in all, researchers really get quite excited about all the positive things gratitude is related to.
There is also research indicating gratitude can help increase resilience and cope with everyday life stress, as well as with more major adversities.
Gratitude can help mental health – for instance, a depressed mood or post-traumatic stress disorder – and with coping well from loss after trauma.
Sign me up. How can I use it this Christmas?
So, if you want to buffer against those annoying relatives, blown budgets and be more resilient to life’s stressors, developing a greater sense of gratitude can help.
Among the many ways researchers have tested, you can:
- write a thank you note for a gift or behaviour you’ve appreciated. It doesn’t have to be a hand written letter. You can express gratitude via text, email or social media
- visit someone and thank them in person
- keep a daily journal of things you feel grateful for, such as noting down three things at the end of the day as well as your role in bringing about the three things
- spend time contemplating being grateful for certain activities, such as having a family or friends to spend Christmas with or opening presents with children. In other words, thinking about being grateful is also helpful, not just the act of being grateful.
Hang on a minute. Surely it’s not that simple
However, there are also a few tricks, twists and turns to be aware of:
- consider cultural nuances: someone’s culture can influence how they perceive and react to gratitude. For example, in East Asian and Indian cultures, receiving gratitude can be accompanied by feelings of indebtedness or guilt. This can put pressure on people to reciprocate. This can also be true, but not to the same extent, in Western cultures
- gratitude is not for everything: gratitude is not the panacea to all stresses of life; it helps, but it does not cure. It should also not be used to distract from real issues and problems, especially in interpersonal relationships
- think about when you use it: be purposeful and strategic about expressing gratitude and don’t overdose on it. Start with the people who help you the most and are the most meaningful to you
- don’t forget yourself: show gratitude towards yourself as well as others, such as being grateful for some of your strengths and capabilities.
If you can’t be grateful …
With all the best will in the world, it can be difficult to be grateful faced with the same present from Aunt Betty three years in a row. In this case, our only advice is to smile, and grin and bear it, rather than to pretend to be grateful. You will feel better and so will she.
Matthew Higgins, who has been admitted to the PhD program at Claremont Graduate University in the United States, co-authored this article.
Interim report on aged care predicts reforms needed
On 31 October 2019 the Royal Commission into Aged Care Quality and Safety released its interim report after 10 months of public inquiries on the aged care industry.
The interim report provides a narrative of the aged care landscape in Australia, structured into three volumes. Volume 1 – which contains the bulk of the report – is set out in three parts:
- Part 1 provides a historical overview of the aged care system and previous inquiries and reforms, and considers demographic, social and economic pressures on the system.
- Part 2 sets out persons’ experiences of the aged care system through direct evidence records and submissions.
- Part 3 highlights several issues in the aged care system, such as the availability of information on aged care services, access to aged care, use of restraints in residential aged care, and recruitment of trained staff.
Volume 2 contains an overview of public hearings conducted by the Commission to-date, and Volume 3 contains appendices and summaries of community forums held by the Commission.
The Commission has not included specific recommendations pending its final report.
Overarching theme
The theme recurring through the Commission’s interim report is that of a system not meeting the needs of the aged population and in need of reform.
The report describes the problems that older persons and their families face in accessing aged care. It also details service shortfalls, the use of restrictive practices in aged care, the experience of the workforce, and highlights the issue of young people living in residential aged care.
What recommendations are likely to be proposed in the final report?
While it is still early days and the Commission’s recommendations will only be published in its final report, the Commission has set out its observations and early conclusions on a number of issues. These are:
- Improving people’s experience in navigating the aged care system and helping them to access the right service. Specifically, the Commission has indicated it will look into improving access to information to enable comparisons of available aged care services, and into improving the availability of information as to the length and progress on home care waiting lists.
- Considering options to address the current waiting times for Home Care Packages, which may include more localised approaches to service planning and allocation; greater transparency of the waiting list; increased flexibility in Home Care Packages; ‘uncapping supply’ of home care; combining home care with home support; and allocation of unspent funds. The Commission has also stated additional funding should be provided for Home Care Packages immediately and into the future, to ensure that supply meets community expectation.
- Improving the provision of aged care for Aboriginal and Torres Strait Islander people so it is delivered in ways that are flexible, adaptable and culturally safe. The Commission will also explore ways to support aged care services to be staffed and managed by Aboriginal and Torres Strait Islander people.
- Making recommendations on changes in the medical and operational practices utilised in residential aged care, to address the prevalence of restrictive practices (particularly the use of chemical restraints).
- Addressing workforce issues, including attracting and retaining staff; education and training; choosing the right staff; remuneration and careers; continuity of care; and staffing levels and staff mix.
- Considering solutions for younger people currently accessing aged care. The Commission has proposed that, subject to very limited exceptions, by 2022 no younger people should be entering residential aged care, and by 2025 no younger people should be living in residential aged care except for those who choose to be there.
Areas for more immediate attention
The Commission also identified three areas for more immediate attention:
- providing more Home Care Packages to reduce the waiting list for higher level care at home;
- responding to the over-reliance on chemical restraints in aged care; and
- stopping the flow of younger people with disability going into aged care and speeding up the process of getting out younger people already in aged care.
Government’s response
The Government has on 25 November 2019 responded to the Commission’s report by pledging a $537 million funding package across the three priority areas identified, which will be used to:
- increase the number of Home Care Packages;
- improve medication management programs to reduce the use of medication as a chemical restraint on aged care residents;
- provide training and support for aged care workers and providers; and
- invest to help meet new targets to remove younger people from aged care.
The Government’s response can be found here: https://www.pm.gov.au/media/response-aged-care-royal-commission-interim-report
What is next?
The Commission’s comments make clear that reforms to all aspects of the aged care industry, and not just the practices of aged care providers, will be proposed in its final report. Indeed, the Commission has flagged that it will ‘recommend comprehensive reform and major transformation of the aged care system in Australia’.
This will be welcome news to applicants facing issues accessing aged care or funding, although details as to how the changes impact them will only be clear when final specific recommendations are published. For aged care service providers, the likelihood of increased regulation and tougher accreditation and service standards following from the inquiry, may result in providers facing increased capital and operating cost requirements. We could potentially see consolidation in the sector and investment opportunities could present themselves for potential investors, as the impact of the Commission becomes clearer over time.
However, the Commission is still midway through its inquiry and implications arising from its inquiry will only be clear when its final report is issued (the final report is due in November 2020). In the meantime, the interim report sends a clear signal that the aged care sector will likely see comprehensive and significant changes over the next few years.
More information about the Aged Care Royal Commission can be found here: https://agedcare.royalcommission.gov.au
A last-minute pressie for someone you know
Climate change and ageing population create ‘a perfect storm’
The combination of climate change and an ageing population is interacting to create “a perfect storm”, according to a research paper written for the Actuaries Institute.
Heatwaves are killing more Australians than any other natural disaster and are expected to become more frequent and last for longer with over-65s particularly at risk.
The paper, The Impact of Climate Change on Mortality and Retirement Incomes in Australia, was written by Ramona Meyricke, a senior actuary and associate investigator, and Rafal Chomik, a senior fellow at the Centre for Excellence in Population Ageing Research at the University of NSW.
These researchers say that deaths from heatwaves could rise by 12 per cent among over 65-year-olds, with heatwaves expected to triple in some regions.
“More frequent, longer and hotter days will drive a significant increase in mortality, with Australia’s ageing population amplifying the number of people who will die as a result of climate change,” the paper says.
It also canvases the financial implications of climate change for investors, warning of long-term negative returns.
The paper examines how climate change will affect Australians in broad ways, including the impact on economic growth, health and mortality, government spending and investment returns. It explores the consequences for individuals and businesses, including health, general and life insurers, pension providers, investors and emergency services and governments.
It states that climate change and ageing populations are interacting to create “a perfect storm”.
“Without proper risk management, these megatrends have the potential to overwhelm individuals, private companies and government balance sheets over the course of this century,” the authors state.
“In terms of public policy, the wide-ranging consequences of climate change on mortality, public health and the economy mean that system-wide policy responses are necessary to mitigate the risks posed.”
Heatwaves have killed more Australians than bushfires, cyclones, earthquakes, floods and severe storms combined, and are the main threat to Australians’ mortality from climate change, the authors say, warning that population ageing is a major contributor to the numbers.
The Australian Bureau of Statistics (ABS) projects that by 2050, the population of over-65s and over-85s will nearly double and triple respectively.
“Population ageing will amplify the burden of heat related mortality and health risks in a warming climate – an interaction that policymakers and insurers have not yet fully taken into account,” the report states.
It says that the potential impact of climate change could also extend to lower superannuation contributions and investment returns due to negative long-term returns for investors whose portfolios are not diversified. This, in turn, could lead to lower superannuation balances.
The predictions also have major implications for pension providers, including the Federal Government. The authors say there may be a greater reliance on the Age Pension if climate change seriously diminishes superannuation balances, and a higher cost of provisioning for future Age Pension liabilities if investment returns are lower.
Have you considered the implications of climate change on your income?
How to get more purpose into your life…